What are the hormones involved?
Women are born with all their follicles at birth and do not develop any more as they get older. These follicles are the source of estrogen and progesterone which are active mainly during her reproductive years. These 2 hormones, estrogen and progesterone are vital in controlling the menstrual cycle and fertility issues. Estrogen is also vital in maintaining various organs in the woman including the brain, skin, heart, and bone.
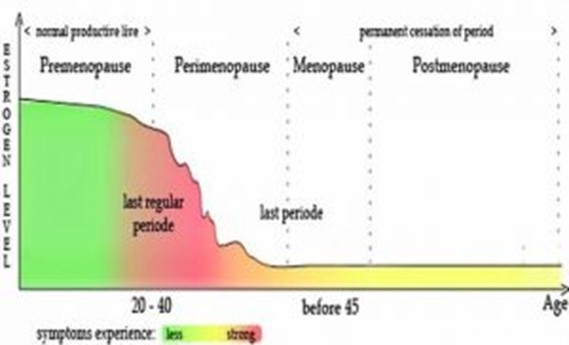
During the menopause, these follicles release less estrogen and progesterone and this is the beginning of menopausal symptoms and changes. When the follicles cease functioning completely, periods stop.
Two other hormones, follicular stimulating hormone (FSH) and luteinizing hormone (LH) are the controllers of estrogen and progesterone. When estrogen and progesterone levels drop, there is loss of control of FSH and LH and these 2 hormone levels start rising. A rising FSH level is the first indicator of impending menopause.
Factors that affect the age of menopause are:
- Current and past history of cigarette smoking. Smoking makes menopause earlier by 2 years. The age of menopause is also affected by passive smoking,
- Family history of early menopause,
- Ethnicity. Menopause occurs earlier in Japanese -American women and Hispanic women when compared to Caucasian women,
- Low body weight,
- Living in high altitudes,
- Vegetarianism,
- Malnourishment in women.
What is the average age of menopause?
The average of menopause around the world is 51 years (50-52 years). In Malaysia, the average age of menopause has been found to be around 50.7 years.
Premature Menopause is having menopause before the age of 40 years. This may happen naturally, surgically (when both the ovaries are removed) or induced (chemotherapy or radiotherapy for malignancies).
Late menopause is when menses goes on beyond the age of 55 years. Women who menopause late may have an increased risk of breast and uterine problems.
Symptoms of Menopause
Here is an almost complete list of symptoms that women may have when they go through menopause.
No one has all these symptoms.
Many women just breeze through this transition whilst others have just a few symptoms that don’t need treatment.
Only women who are unable to cope with these symptoms need medical treatment.
- Irregular periods: A variation in their period cycles. Shorter and lighter periods, longer cycles sometimes heavy periods with flooding, prolonged periods, painful periods.
- Hot flushes: sudden explosions of heat starting at the chest moving up to the face. It just last seconds and may be followed by sweating.
- Night sweats: when hot flushes happen at night followed by episodes of sweating. There can also be cold sweats and clammy sensations.
- Irregular heart beats
- Anxiety especially at night which adds on to palpitations and gastric pain.
- Irritability, temper tantrums, mood swings, tearfulness.
- Feeling of doom, dread and depression. Women who have more intense premenstrual mood swings and post-natal blues and depression, have a higher chance of menopausal depression.
- Difficulty in concentration. Mental disturbances and mental confusion.
- Memory lapses, forgetfulness.
- Sleep disturbances, light sleep, disturbed sleep all adding on to tiredness the next morning.
- Loss of libido. No mood for sex and sexual pleasures.
- Dry vagina and loss of lubrication. This causes painful sexual activity which when added on to loss of libido makes a woman turn of sex completely. She may even experience chaffing of the vaginal skin, burning and tearing and bleeding of the vaginal tissue.
- Inability to control bladder, leading to incontinence especially when laughing, or sneezing. This is due to loss of muscle tone of the bladder.
- Extreme tiredness with no energy to do routine tasks. Finds it unable to get through the day. Restlessness and listlessness.
- Dry skin leading to itchiness and sensation of ants crawling. There can also be eye dryness and mouth dryness.
- Thinning of skin causing wrinkles and sagging of skin
- Increase in pigmentation especially over the face.
- Increased in small skin tags over the body.
- Aching muscles, joint pains, creaking joints and generalised body pain
- Breast tenderness and soreness.
- Headaches usually increasing in intensity may be secondary to sleep disturbances.
- Bloating and stomach disturbances. Flatulence and burping.
- Weight gain and lowered metabolism. It is usually the midriff area where the weight piles on.
- Increased sensitivity to certain foods that did not give problems before. Such as dairy products, gluten and wheat.
- New allergies to medication that was safe before.
- Start of medical conditions such as diabetes, high blood pressure and cholesterol.
- Pre-existing medical conditions worsen such as diabetes, hypertension and cholesterol.
- Increased risk of coronary heart disease.
- Changes in thyroid levels.
- Hair loss or thinning, whitening of hair and increase in facial hair.
- Changes in body odour with bad breath.
- Dizziness, light-headedness and imbalance. Ringing in the ears.
- Tingling sensation over any part of body and under the skin.
- Gum issues with loosening of teeth and bleeding gums.
- Bone loss and osteoporosis.
- Changes in nails – softer and more brittle..
If I have these symptoms, does it mean that menopause is around the corner?
Symptoms of menopause usually occur in the 40s when the estrogen levels start going down. However some women begin experiencing these symptoms even in their 30s even though the actual last period may be at 50.
Recommendations
The woman in the menopausal transition goes though physical, mental, emotional and health changes. Primary prevention or early detection of health issues is important and should be emphasized. Key lifestyle changes in diet and exercise, maintaining ideal body weight, being proactive about regular health checkups, carrying our regular mammograms and targeted investigations as deemed necessary (such as DEXA bone density screening) help ease the changes into the postmenopausal era.
Menopausal Hormone therapy (MHT) should be encouraged for the younger postmenopausal woman with moderate to severe vasomotor symptoms. A risk-benefit assessment should be carried out prior to its commencement and at regular intervals thereafter.
Non hormonal treatment for vasomotor symptoms is available. Vaginal estrogen creams which have minimal systemic absorption is available for vaginal and bladder problems especially dryness and atrophy. MHT helps improve BMD (bone mineral density) and treat osteoporosis but should not be considered as the first line therapy for the osteoporotic woman. The risk of MHT on cancers should be carefully evaluated against the background risk of the individual woman.
Menopausal Hormone Therapy
Women who are unable to cope with menopausal symptoms to the extent that it interferes with quality of life can consider Menopausal Hormone Therapy (MHT). MHT was at one time referred to as HRT (hormone replacement therapy).
Replacing the lost estrogen that occurs with menopause helps women cope with their symptoms better. Estrogen is replaced either in the form of tablets, patches or creams.
Women who have had their uterus taken out for various reasons, need only take estrogen hormones.
Estrogen is always combined with progestins when a woman has her uterus intact. In such women, taking estrogen alone, can increase the thickness of the lining of her uterus and cause bleeding problems, hyperplasia (over activity of the uterine lining) or even cancer of the uterus in the future.
Women who have their uterus intact need estrogen and at least 10 -12 days of progestins every month.
Before prescribing HT, your doctor would probably take a good history and carry out a gynaecological examination. It would be good to provide a detailed family history of cardiovascular disease, migraines, deep vein thrombosis, cancers and osteoporosis. Blood pressure values, height and weight measurements and BMI would be tabulated.
A pap smear (where relevant), a pelvic ultrasound and mammography is ideal as baseline investigations and again at regular intervals. Bone mineral density tests is encouraged for women with a high risk of fracture.
Your doctor would then carry out a risk / benefit assessment based on your symptoms, your health and existing medical and family history.
Benefits of MHT
- Relief of vasomotor symptoms such as hot flushes, night sweats, tiredness, aches and pains, mood swings, sleep problems etc.
- Improvement in energy levels.
- Improvement in dryness of skin.
- Improvement in quality of hair.
- Improvement in urogenital symptoms leading to better vaginal health, less pain during sexual activity and lesser risk of infections of the bladder and vagina.
- Improvement in libido.
- Decreases risk of recurrent urine infections and improves urinary incontinence.
- Decrease in total cholesterol and LDL (bad cholesterol) levels. This improves the cardiovascular status of the heart and decreases risk of heart blocks (atherosclerosis). Non oral HT has been shown to be more beneficial to the heart.
- Improvement of bone density and decrease in fracture risk.
- Improvement in balance and reduces tendency to fall.
- Decreases risk of osteoarthritis.
- Improvement in quality of health.
- Decreases risk of diabetes mellitus.
- Decreases risk of colorectal cancer.
- Decreases risk of breast cancer in women (without a uterus) who only take estrogen.
- Preserves teeth with a lesser risk of osteoporosis of jaw.
- Decreases risk of cataract formation, dry eyes and age related macular degeneration.
MHT does not help in
- Improvement of memory.
- Age related dementia or degeneration.
- Improvement in Alzheimer’s disease.
Risks of MHT
- Stroke risk. A very small increased risk of stroke in both combined HT and estrogen only users who take hormones orally. Non oral HT users have no increased risk of stroke.
- Venous thromboembolism (VTE) or clots in the blood vessels: A very small increased risk in oral users of estrogen and combined HT users. No increased risk of VTE in non-oral HT users.
- Breast cancer: A very small increase which equates to 6.8 additional cases per 1000 women per five years for combined HT users. No increased risk in estrogen only users if used for less than 6 years.
- Small increase in gall bladder disease.
- A small increase in flares if the post menopausal woman has systemic lupus erythromatosis (SLE).
There is no increased risk of lung or ovarian cancer
Your doctor would also not put you on hormone therapy if
- you have breast cancer
- you are pregnant
- have a estrogen dependant cancer
- have abnormal vaginal bleeding
- have history of clotting problems
- have had bad reactions to hormone therapy in your past
Side Effects of HT
It is quite common for the body to take time to adjust to the hormones in your body. The common side effects are breast tenderness, bloating, headaches, nausea. To lessen these effects, the dose of MHT can be changed or the delivery method could be fine tunes.
Many women are worried about weight gain. However a meta-analysis of 28 trials found no evidence of increase in weight or body mass index with either estrogen only use or estrogen / progestin use.
An increase in pigmentation may occur but allergic reactions are rare.
Duration of Use
The two main factors that have questioned the duration of use of MHT is the increased risk of breast cancer and the effect of MHT on coronary heart disease.
Breast Cancer
Combined MHT ( in women with an intact uterus) users showed a higher risk of breast cancer and breast cancer mortality after 4-5 years of use in the WHI (Women’s Health Initiative) study, while the estrogen only users did not show any increased risk after 6 years of continuous use.
Coronary heart disease (CHD)
Younger post-menopausal women on both estrogen / progestin (combined MHT) do not show an increased risk of cardiovascular, stroke or VTE risk.
The younger post menopausal woman (50-59 years) on estrogen only MHT showed a significantly lower risk of CHD and heart attacks (myocardial infarction).
General recommendations advice that MHT use is safe in the younger menopausal woman (within 10 years of menopause).
There is presently no time limit for the duration of MHT use.
Every woman on MHT should be regularly followed up and should have a risk/ benefit assessment carried out yearly.
 Malaysia
Malaysia